Saskatchewan could see anywhere from 3,000 to over 8,000 deaths from COVID-19, even with current preventative measures in place, modelling from the province shows.
The data, released Wednesday, shows a variety of possible scenarios, from no action taken to a low range of spread.
The modelling is based on scenarios and is not a prediction, the province emphasized. Officials stressed that it’s too early to make a prediction, and the province doesn’t know where it is on the curve. They can only hope measures taken so far have been successful.
The analysis is based on three scenarios of infected patients spreading the virus to an average of four others each, based on early Canadian estimates, 2.76 people each based on the low-Italy spread and 2.4 people each, based on spread in Wuhan, China, where the virus originated.
The analysis suggests that at its peak, there could be anywhere from 60 hospital admissions per day (based on the low-range of spread) to 710 per day based on the high level of spread.
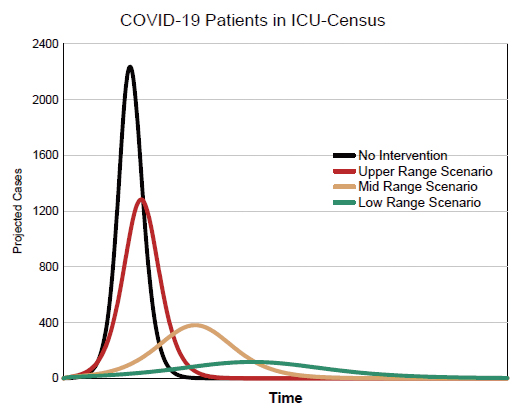
The total number of cases ranges from 153,900 to 408,000 and the number of patients requiring ventilation and ICU from 120 to over 1,200.
If no social distancing measures were taken, the projections show even more dire results.
Graphs included with the provincial reports show that without intervention, cumulative COVID-19 cases would approach 500,000 and deaths would near the 10,000 mark.
The province teamed up with Dr. Nathanial Osgood and the computational epidemic epidemiology and public health informatics lab at the University of Saskatchewan. Osgood has been modelling potential pandemic outbreak scenarios since the virus took hold in Wuhan months ago. The province’s modelling was also reviewed by national-level researchers.
The modelling, the province notes, is not a prediction. Rather, it provides a range of “what if” scenarios to guide planning.
“Current interventions have made a difference,” the document says. “The most important variable to save lives and protect health care workers is public compliance with isolation measures, physical distancing and washing your hands.”
Since COVID-19 is new, there is no experience in the past that specifically speaks to the Saskatchewan situation.
“The dynamic modelling allows us to look at learning that we have fro mother jurisdictions and the evidence that’s coming through to really look at how could COVID-19 transmit in our population, what would be the impact be of various public health interventions and the subsequent impact on acute care demand,” said Dr. Jenny Basran, Senior Medical Information Officer.
It’s too early on in the pandemic to know where Saskatchewan sits on that curve, she explained.
“It is too early for us to know the exact scenario that we’re in in Saskatchewan and it will really depend on how Well, we are complying with the chief medical health officer interventions. Our hope is that we are on a better trajectory than our ‘what if’ scenarios, but at the current time, we do not have enough information to be able to now for certain.”
In other jurisdictions, she said, when medical systems weren’t prepared for the worst, the rate of deaths from the virus and from other untreated illnesses increased.
“It’s critical to remember that this data is not a prediction for the future,” said SHA CEO Scott Livingstone during a media briefing.
“It’s data that acts as a planning tool to ensure that we’re preparing for the worst, but aiming for the best. What we do know at this point is that our health system strategy for COVID-19 has already paid dividends. Public health measures are already starting to show encouraging signs of flattening the curve. … But to ensure that we’re prepared for the worst-case scenario, we need to do more.”
The province is planning both an offensive and defensive approach to containing the virus.
The offence is about containment and delay. The defence is about mitigation, or ensuring services are available when needed.
“We are all playing for the same team,” the province writes.
‘We win and lose together. No health system in the world can withstand this pressure without sustained help from the public.”
The province’s offensive strategy includes increasing testing, identifying cases early and expanding contact tracing capacity, along with enforcing public health orders.
So far, 38 SHA-operated testing sites have been established across the province. There are five assessment sites in operation, with 21 more to follow in the coming weeks.
The province lists its strategies as prioritizing testing protecting health care workers and first responders, screening in long-term care, partnering with communities and across sectors and ensuring messaging for health education, health promotion and health equity.
“We need to remember: these measures must be sustained to be effective,” the document says.
“We need to keep learning, understanding and removing barriers that prevent people from taking necessary action. The COVID-19 global pandemic will continue for weeks and months to come — we may not see the whole picture or understand its full impact until it’s over.”
The defensive strategy is about meeting the care needs of the province while minimizing the loss of life.
Still, the strategy notes, the continuity of essential and urgent health services for non-COVID-19 patients needs to be maintained.
The province is planning a staged response as demand rises
That includes different use of different health facilities in different parts of the province with a centralized bed flow coordination service.
Staff and physicians may be deployed to other facilities to support care.
So far, a slowdown of non-essential and non-urgent services has freed up more than 1,000 beds.
The province is planning to phase in 57 per cent more acute beds as needed and increasing intensive care beds from 98 to 963 as needed.
The planned capacity is based on an estimate of patient demand between the high and mid-range modelling scenarios.
Contingency plans are based on a higher-range estimate of patient demand.
The planned capacity includes a gap of 410 ventilators. The province has ordered 200, with 100 expected in the next two to three weeks. The provicne said it does have enough ventilators for its low-range projections.
In the Integrated Northern Health area, which includes prince Albert, there will be no facility closures and no COVID-only hospitals.
Some hospitals, such as those in Shellbrook, Rosthern, Tisdale and Porcupine Plain, will be for non-COVID patients only. Other hospitals, such as Prince Albert, Melfort, Nipawin, La Ronge and La Loche, will see a mixed patient cohort. Contingency plans could see a COVID-only hospital open in the region, but that’s only for the direst scenario, not the one that’s leading the health system’s plan.
“We will be cohorting COVID-19 patients on designated units within facilities,” explained Derek Miller, the Emergency Operations Centre lead. he added that the health system will manage its load levels to ensure that there isn’t one health facility overloaded and patients are spread out across the system.
“This is a provincial response is not by facility or siloed within areas or geographies,” Miller continued.
“We are going to manage this through centralized bed flow coordination, air traffic control-like coordination of patients to ensure that they are seeking and getting care in the right and best locations.”
The southern part of the province will have hospitals solely dedicated to COVID-19 stood up based on demand.
In Saskatoon and Regina, field hospitals are planned to deal with the surge — one at Merlis Belsher Place and one at Evraz Place. Additional capacity is also being created in acute care and ICU settings to prepare for the surge.
The province outlined its modelling scenarios during a press conference Wednesday. Regional information will be made available tomorrow.
The full modelling document is available below:
Health-System-Readiness-for-COVID-191
